BMA responds to rapid review into gross negligence manslaughter
| Response comes in the aftermath of the Dr Bawa-Garba ruling
Related items from OnMedica Bawa-Garba case: was the GMC biased? |
Powered by WPeMatico
| Response comes in the aftermath of the Dr Bawa-Garba ruling
Related items from OnMedica Bawa-Garba case: was the GMC biased? |
Powered by WPeMatico

A few new drugs have been approved by the FDA so far this year. Among them are treatments for cystic fibrosis, prostate cancer, pancreatic cancer, and two new treatments for HIV.
Symdeko from Vertex is a combination of tezacaftor and ivacaftor for the treatment of cystic fibrosis in patients age 12 years and older. Tezacaftor is a cystic fibrosis transmembrane conductance regulator (CFTR) corrector. Ivacaftor is a CFTR potentiator.
Symdeko is specifically indicated for the treatment of patients with cystic fibrosis (CF) aged 12 years and older who are homozygous for the F508del mutation or who have at least one mutation in the cystic fibrosis transmembrane conductance regulator (CFTR) gene that is responsive to tezacaftor/ivacaftor based on in vitro data and/or clinical evidence.
The recommended dose of Symdeko is one tablet (tezacaftor 100 mg/ivacaftor 150 mg) taken in the morning and one tablet (ivacaftor 150 mg) taken in the evening, approximately 12 hours apart. The tablets should be swallowed whole. Symdeko should be taken with fat-containing food.
Adverse effects associated with the use of Symdeko may include, but are not limited to:
Erleada from Janssen Oncology was approved in February to treat a certain type of prostate cancer using novel clinical trial endpoint. Erleada works by blocking the effect of androgens, a type of hormone, on the tumor. These androgens, such as testosterone, can promote tumor growth.
“The FDA evaluates a variety of methods that measure a drug’s effect, called endpoints, in the approval of oncology drugs. This approval is the first to use the endpoint of metastasis-free survival, measuring the length of time that tumors did not spread to other parts of the body or that death occurred after starting treatment,” said Richard Pazdur, M.D., director of the FDA’s Oncology Center of Excellence and acting director of the Office of Hematology and Oncology Products in the FDA’s Center for Drug Evaluation and Research. “In the trial supporting approval, Erleada had a robust effect on this endpoint. This demonstrates the agency’s commitment to using novel endpoints to expedite important therapies to the American public.”
Adverse effects associated with the use of Erleada may include:
Advanced Accelerator Applications has recently received FDA approval for Lutathera to treat a type of cancer that affects the pancreas or gastrointestinal tract called gastroenteropancreatic neuroendocrine tumors (GEP-NETs). Lutathera (lutetium Lu 177 dotatate) is a radiolabeled somatostatin analog.
Lutathera is supplied as an injection for intravenous administration. The recommended dose is 7.4 GBq (200 mCi) every 8 weeks for a total of 4 doses.
Adverse effects may include, but are not limited to, the following:
Biktarvy from Gilead was approved in February for the treatment of HIV-1 infection in adults.
Biktarvy is specifically indicated as a complete regimen for the treatment of HIV-1 infection in adults who have no antiretroviral treatment history or to replace the current antiretroviral regimen in those who are virologically suppressed (HIV-1 RNA <50 c/mL) on a stable antiretroviral regimen for at least three months with no history of treatment failure and no known substitutions associated with resistance to the individual components of Biktarvy.
Biktarvy is supplied as a tablet for oral administration. The recommended dose is one tablet once daily with or without food.
Adverse events associated with the use of Biktarvy may include:
TaiMed Biologics has received FDA approval for Trogarzo to treat HIV patients who have tried multiple HIV medications in the past and whose HIV infections cannot be successfully treated with other currently available therapies (multidrug resistant HIV, or MDR HIV). This antiretroviral medication is administered once every 14 days and used in combination with other limited antiretroviral medications.
“While most patients living with HIV can be successfully treated using a combination of two or more antiretroviral drugs, a small percentage of patients who have taken many HIV drugs in the past have multidrug resistant HIV, limiting their treatment options and putting them at a high risk of HIV-related complications and progression to death,” said Jeff Murray, M.D., deputy director of the Division of Antiviral Products in the FDA’s Center for Drug Evaluation and Research. “Trogarzo is the first drug in a new class of antiretroviral medications that can provide significant benefit to patients who have run out of HIV treatment options. New treatment options may be able to improve their outcomes.”
Adverse effects associated with the use of Trogarzo may include:

The temperature outside may not feel like Spring, but our clocks have moved forward and our days are getting longer. You may be cleaning out closets and doing your annual window washing, but are you taking the time to clean out your medicine cabinet, too?
In 1979, the U.S. Food and Drug Administration (FDA) began requiring an expiration date on prescription and over-the counter medicines. “The medicine expiration date is a critical part of deciding if the product is safe to use and will work as intended,” says Ilisa Bernstein, Pharm.D., J.D., Deputy Director of the Office of Compliance in FDA’s Center for Drug Evaluation and Research. The expiration date can be found printed on the label or stamped onto the bottle or carton, sometimes following “EXP.” It is important to know and stick to the expiration date on your medicine. Using expired medical products is risky and possibly harmful to your health.
Expired medications can be less effective or risky due to a change in chemical composition or a decrease in strength. Certain expired medications are at risk of bacterial growth, and sub-potent antibiotics can fail to treat infections, leading to more serious illnesses and antibiotic resistance. “Once the expiration date has passed there is no guarantee that the medicine will be safe and effective,” says Bernstein. “If your medicine has expired, do not use it.”
In addition, many Americans may not be not aware that medicines that sit in their medicine cabinets are highly susceptible to diversion, misuse, and abuse. With the rise of prescription drug abuse in the United States, the number of accidental poisonings and overdoses has dramatically increased. Oftentime, the abused prescription drugs are unknowingly obtained from family and friends, whether taking medications out of a purse, or a home medicine cabinet.
Finally, expired medicines are also not just a risk to the person they were prescribed for —they can injure children and pets if taken by mistake. For all these reasons, proper disposal of unneeded and expired medicines is essential!
First, read the medicine’s label and follow any specific disposal instructions that may be included. A drug take-back program, if available, is the preferred way to dispose of expired, unwanted or unused medicine. From 10am – 2pm on April 28th at Village Pharmacy in Hampstead, we are participating in the National Prescription Drug Take-Back Day. The event addresses a vital public safety and public health issue by focusing attention on the importance of keeping your communities safe and reminding everyone to get rid of unneeded and outdated medicines. Through this important program many tons of unneeded and out-date drugs have been removed for proper disposal.
When drug take-back programs aren’t available, federal guidelines recommend throwing the medicines away in the household trash after mixing them with a substance like dirt or kitty litter and then sealing the mixture in a container like a zipper baggie.
Follow these instructions for disposing of most medications in the household trash:
For a list of medicines recommended for disposal by flushing, as well as other information on proper disposal, please see the FDA’s Disposal of Unused Medicines page.
Proper storage is one way to help make sure your medicines will remain safe and effective up to their expiration date. Be sure to read the label to see if there are specific storage instructions for your medicine. Certain medicines need to be stored in the refrigerator and others cannot be exposed to high temperatures. Improper storage – such as a damp bathroom cabinet – can contribute to decreased effectiveness in medicines that have not reached their posted expiration date. For most medicines, to help ensure the proper shelf life of your medicine, it is better to store medicine in a cool, dry place such as a dresser drawer, storage box, closet shelf, or kitchen cabinet.
When storing medicine in a kitchen cabinet make sure that it is away from hot appliances and the sink due to changing temperatures and humidity, which can affect the medicine. When storing medicine in a high traffic area, like a kitchen, care should be taken to prevent access by children at risk of accidental poisoning or others who may be tempted to take for abuse/misuse.
Remember to store medicines properly and don’t use expired medicines — it’s not worth the risk!
Hope to see you on April 28th!
Source: FDA and WebMD

Did you know that poisoning is the #1 cause of injury-related death in the U.S.? While the majority of unintentional poisoning deaths in the United States are attributable to misuse and abuse of drugs, environmental substances, such as carbon monoxide and pesticides, also contribute to the poisoning illnesses and deaths occurring in the United States each year. Carbon monoxide causes the most non-drug poisoning deaths (approximately 524 per year), especially among people over 65 years old and males. The majority of pesticide poisoning exposures are unintentional and occur in children under 6 years old or in adults over 20 years old.
A poison is a substance that can cause illness, injury, or death. Poisons can be swallowed, inhaled, or absorbed through the skin. Some substances are toxic in small doses, but other usually harmless substances can be poisonous if encountered in large enough quantities.
Childhood poison exposures often occur as a result of exploratory behavior. In these cases, the amounts ingested are usually small and the health effects minimal. However, exposures to some medicines and household chemicals even in small amounts can result in serious illness or death.
Adult poisonings, on the other hand, are usually drug-related and result from:
Overall, the majority of unintentional poisoning deaths in the United States are attributable to misuse and abuse of drugs. In recent years, deaths involving prescription narcotic painkillers (e.g., oxycodone, hydrocodone, methadone), have outnumbered the combined total of deaths involving the illegal drugs heroin and cocaine.
How do you prevent drug poisoning?
Some household cleaning and lawn care products also contain chemicals that can be poisonous to people. Follow these warning to prevent accidental poisoning:
Carbon monoxide is an odorless, colorless and tasteless gas, and is known as the “silent killer”. If you have an oil or gas heating system, water heater or other fuel burning appliance in your home, follow these tips to keep you safe:
What to do if a poisoning occurs?
Sources: CDC and eMedicineHealth
Colorectal cancer is cancer that starts in the colon or rectum. The colon and the rectum are parts of the large intestine, which is the lower part of the body’s digestive system. During digestion, food moves through the stomach and small intestine into the colon. The colon absorbs water and nutrients from the food and stores waste matter (stool). Stool moves from the colon into the rectum before it leaves the body.
Most colorectal cancers are adenocarcinomas (cancers that begin in cells that make and release mucus and other fluids). Colorectal cancer often begins as a growth called a polyp, which may form on the inner wall of the colon or rectum. Some polyps become cancer over time. Finding and removing polyps can prevent colorectal cancer.
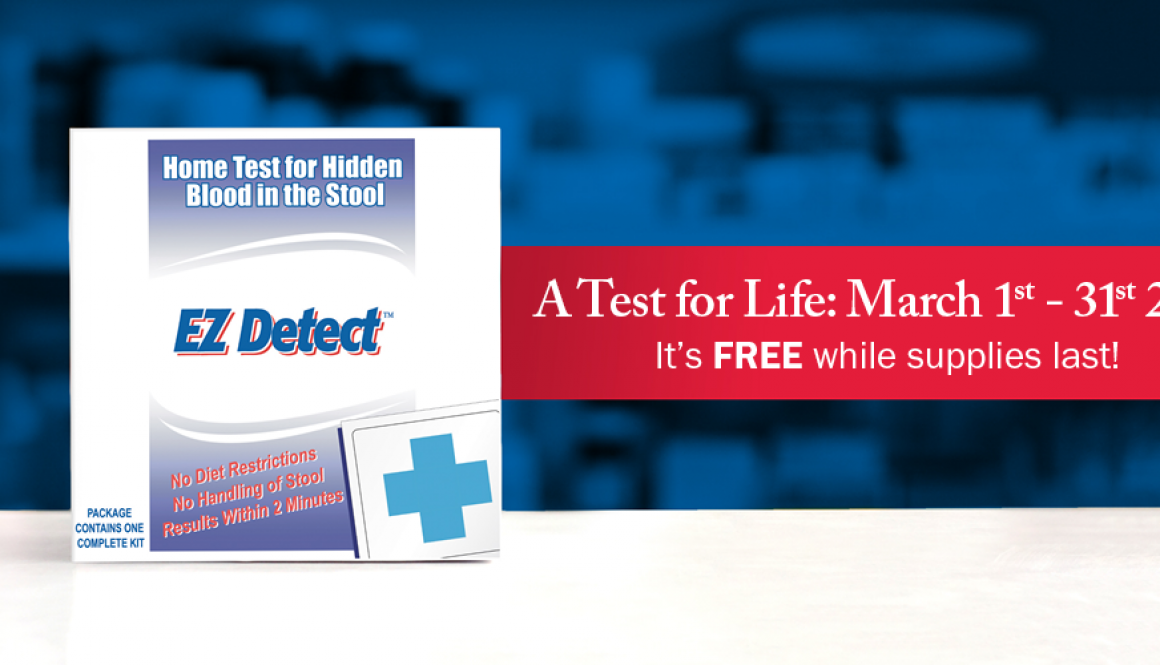
Colorectal cancer is the fourth most common type of cancer diagnosed in the United States. Deaths from colorectal cancer have decreased with the use of colonoscopies and fecal blood tests, which check for blood in the stool.
Older age is a main risk factor for most cancers. The chance of getting cancer increases as you get older Other risk factors for colorectal cancer include:
Signs and symptoms of colorectal cancer include:
Colorectal cancer treatment and chance of recovery depends on the size, location, and how far the cancer has spread. Common treatments include surgery to remove the cancer, chemotherapy, and radiation therapy. However, researchers have been working for decades on finding new treatments to improve patient outcomes. These efforts include the development of more effective—and less toxic treatments—such as targeted therapies, immunotherapies, and cancer vaccines. Further development of chemotherapy, radiation therapy and surgery are also being improved. Some studies are working to improve the patient’s ability to receive effective cancer treatment by managing the treatment’s toxic effects.
By having a better understanding about how specific types of tumors grow, researchers are able to develop targeted therapies and immunotherapies to expand treatment options available to patients with certain types of cancer.
An important part of the research process is patient participation in clinical trials. If joining a clinical trial is a treatment option you’d like to consider, the best place to start is to talk with your doctor or another member of your health care team. Often, your doctor may know about a clinical trial that could be a good option for you. He or she may also be able to search for a trial for you, provide information, and answer questions to help you decide about joining a clinical trial.
Some doctors may not be aware of or recommend clinical trials that could be appropriate for you. If so, you may want to get a second opinion about your treatment options, including taking part in a clinical trial.
If you decide to look for trials on your own, the following steps can guide you in your search. This information should not be used in place of advice from your doctor or other members of your health care team. This guide takes you through the following steps:
Source: National Cancer Institute
There’s a new number for high blood pressure and it’s lower than you think.
For decades the numbers that defined high blood pressure were 140/90 mm Hg. But this past November, the American Heart Association (AHA) and the American College of Cardiology (ACC) issued new comprehensive guidelines that indicate high blood pressure should be treated at 130/80 mm Hg. High blood pressure accounts for the second largest number of preventable heart disease and stroke deaths, second only to smoking. It’s known as the “silent killer” because often there are no symptoms, despite its role in significantly increasing the risk for heart disease and stroke.
In the largest study to date, the Systolic Blood Pressure Intervention Trial (SPRINT) began in 2009 and included more than 9,300 participants, recruited from about 100 medical centers and clinical practices from across the United States. The study was designed to determine the best way to treat blood pressure in adults with hypertension, 50 years or older, who are at a high risk for heart disease.
What does this mean?
This means that instead of 1 in 3 (32%) U.S. adults having high blood pressure, now nearly half (46%) of U.S. adults now are defined as having high blood pressure. That’s 14% more adults have hypertension than previously thought. However, the impact of the new guidelines is expected to be greatest among younger people. The prevalence of high blood pressure is expected to triple among men under age 45, and double among women under 45 according to the report.
“Damage to blood vessels begins soon after blood pressure is elevated”, said Dr. Paul Whelton, who is the Show Chwan professor of global public health at Tulane University School of Public Health and Tropical Medicine and School of Medicine in New Orleans. “If you’re only going to focus on events, that ignores the process when it’s beginning. Risk is already going up as you get into your 40s.”
This does not mean that everyone will—though some will— be prescribed medication to lower their blood pressure. This simply means that people will be counseled about changes in lifestyle much earlier than previously advised.
Paul K. Whelton, M.B., M.D., M.Sc., lead author of the guidelines published in the American Heart Association journal, Hypertension and the Journal of the American College of Cardiology, noted the dangers of blood pressure levels between 130-139/80-89 mm Hg. “You’ve already doubled your risk of cardiovascular complications compared to those with a normal level of blood pressure,” he said. “We want to be straight with people – if you already have a doubling of risk, you need to know about it. It doesn’t mean you need medication, but it’s a yellow light that you need to be lowering your blood pressure, mainly with non-drug approaches.”
Blood pressure categories in the new guideline are:
The new guidelines eliminate the category of prehypertension, which was used for blood pressures with a top number (systolic) between 120-139 mm Hg or a bottom number (diastolic) between 80-89 mm Hg. People with those readings now will be categorized as having either Elevated (120-129 and less than 80) or Stage I hypertension (130-139 or 80-89).
Previous guidelines classified 140/90 mm Hg as Stage 1 hypertension. This level is classified as Stage 2 hypertension under the new guidelines.
Other changes in the new guideline include:
The successful implementation of these guidelines will lead to improvements in the health of the nation and reduce the risks posed by heart disease and stroke. Stop by one of our pharmacies to get your blood pressure checked and do a medication review. We want to make sure you are taking the right medication and we may recommend you see your doctor if your blood pressure is elevated or if you have other conditions that may affect treatment of hypertension.
Sources: American Heart Association and National Institute of Health.
In October 2017, the FDA approved a new shingles vaccine, called Shingrix. In January of this year, the CDC officially recommended that adults 50 and over get the new vaccine to prevent this painful, blistering disease instead of the previous one, Zostavax.
Shingles is an infection of an individual nerve and the skin surface that is supplied by the nerve. It is caused by the varicella-zoster virus, the same virus that causes chickenpox. Anyone who has recovered from chickenpox can develop shingles. There are an estimated 1 million cases of shingles each year in the United States, with 1 in 3 people developing shingles during their lifetime.
Healthy adults 50 years and older are recommended to get two does of Shingrix, two to six months apart. The second dose is really important for long-term protection.
If you have already gotten the Zostavax vaccine, you should now get Shingrix as well. Officially, the CDC states that Shingrix is the preferred vaccine over Zostavax. Even if you’ve had shingles, you should get the Shingrix vaccine, since shingles has been known to reoccur.
What’s the difference between Shingrix and Zostavax?
Shingrix is more than 90% effective at preventing shingles and a patient complication called postherpetic neuralgia (PHN) in all age groups. Conversely, Zostavax is only 51% effective against shingles and 67% against PHN.
Zostavax contains a live, but weakened version of varicella zoster—the virus that causes shingles and chickenpox.
Shingrix has a dead version of the zoster virus. It also contains an adjuvant which causes your body to produce more antibodies to fight shingles than Zostavax.
The CDC recommends getting the Shingrix vaccine when your chances of contracting shingles rises. Initial studies indicate that its protection remains strong for at least four years, but researches hope it will last much longer because the immune response is stronger.
Who should get the Shingrix vaccine?
The CDC says healthy adults ages 50 and over should get the Shingrix vaccine, even if you’re not sure if you ever had chickenpox.
The CDC also recommends that you get the Shingrix vaccine if you’ve already had Zostavax, because it’s more effective. However, you should wait at least two months after you have Zostavax to get Shingrix.
If you’ve already had shingles, you should get the vaccine. The Shingles can come back after you’ve had it.
Who shouldn’t get Shingrix?
Anyone who has had a severe allergic reaction to any of the ingredient in Shingrix should not get the vaccines.
Anyone who has tested negative for immunity to the varicella zoster virus. If you test negative, you should get the chickenpox vaccine.
If you currently have shingles, you should wait to get the vaccine. This can prevent a second bout with the disease.
If you are pregnant or breastfeeding, you should wait to get Shingrix.
The CDC’s Advisory Committee on Immunization Practices hasn’t confirmed whether the vaccine is safe for people who have a weakened immune system because of a disease or medicine they take. One worry is that taking drugs that weaken the immune system might make the shingles vaccine less effective. It’s also possible that by stimulating the immune system, Shingrix could worsen certain diseases, like leukemia.
What are the side effects of the vaccine?
About 1 out of 10 people said the side effects were severe enough to disrupt their daily life. Yet most felt better within 3 to 5 days.
These side-effects are minimal compared the pain and potentially blistering rash caused by shingles where a typical episode can last from 2-4 weeks.
Once the Shingrix vaccine is available, we’ll let everyone know. Then you can stop by one of our pharmacies and get your shot. We want to keep you healthy!
Sources: CDC, Web MD and Consumer Reports
We’ve all heard that smoking increases the risk of many life-threatening diseases—including lung cancer, emphysema, and heart disease. But did you know that smoking also contributes to many cancers and diseases of the digestive system? Estimates show that about one-fifth of all adults smoke, and each year at least 443,000 Americans die from diseases caused by cigarette smoking.
Smoking has been found to increase the risk of cancers of the:
Research also suggests that smoking may also increase the risk of cancers of the liver, colon and rectum.
What are the other harmful effects of smoking on the digestive system?
Smoking contributes to heartburn, gastroesophageal reflux disease (GERD), peptic ulcers, and some liver disease. Smoking increases the risk of Crohn’s disease, colon polyps, and pancreatitis, and it may increase the risk of gallstones.
Heartburn is the painful, burning feeling in the chest caused by reflux. Smoking weakens the lower esophageal sphincter, the muscle between the esophagus and stomach that keeps stomach contents from flowing back into the esophagus. This causes heartburn and can possibly damage the lining of the esophagus.
GERD is persistent reflux can can lead to serious problems such as bleeding ulcers of the esophagus, narrowing of the esophagus that causes food to get stuck, and changes in the esophageal cells that can lead to cancer.
Peptic Ulcers
Smoking increases the risk of peptic ulcers. Peptic ulcers are sores on the inside lining of the stomach. The two most common causes of peptic ulcers are infection with a bacterium called Helicobacter pylori (H. pylori) and long-term use of nonsteroidal anti-inflammatory drugs such as aspirin and ibuprofen.
Studies suggest that smoking increases the risk of H. Pylori infection, slows the healing of peptic ulcers, and increases the likelihood that peptic ulcers will recur. Smoking increases the production of substances that may harm the lining of the stomach and the duodenum (the first part of the small intestine). Smoking also decreases factors that protect or heal the lining including:
Liver Disease
The liver is the largest organ in the digestive system. The liver carries out many functions, such as making important blood proteins and bile, changing food into energy, and filtering alcohol and poisons from the blood. Research has shown that smoking harms the liver’s ability to process medications, alcohol, and other toxins and remove them from the body. In some cases, smoking may affect the dose of medication needed to treat an illness.
Smoking may worsen some liver diseases, including:
Crohn’s Disease
Current and former smokers have a higher risk of developing Crohn’s disease than people who have never smoked.
Crohn’s disease is an inflammatory bowel disease that causes irritation in the GI tract. The disease, which typically causes pain and diarrhea, most often affects the lower part of the small intestine; however, it can occur anywhere in the GI tract. The severity of symptoms varies from person to person, and the symptoms come and go. Crohn’s disease may lead to complications such as blockages of the intestine and ulcers that tunnel through the affected area into surrounding tissues. Medications may control symptoms. However, many people with Crohn’s disease require surgery to remove the affected portion of the intestine.
Among people with Crohn’s disease, people who smoke are more likely to:
The effects of smoking are more pronounced in women with Crohn’s disease than in men with the disease.
Researchers are studying why smoking increases the risk of Crohn’s disease and makes the disease worse. Some researchers believe smoking might lower the intestines’ defenses, decrease blood flow to the intestines, or cause immune system changes that result in inflammation. In people who inherit genes that make them susceptible to developing Crohn’s disease, smoking may affect how some of these genes work.
Colon Polyps
People who smoke are more likely to develop colon polyps. Colon polyps are growths on the inside surface of the colon or rectum. Some polyps are benign, or noncancerous, while some are cancerous or may become cancerous.
Among people who develop colon polyps, those who smoke have polyps that are larger, more numerous, and more likely to recur.
Pancreatitis
Smoking increases the risk of developing pancreatitis. Pancreatitis is inflammation of the pancreas, which is located behind the stomach and close to the duodenum. The pancreas secretes digestive enzymes that usually do not become active until they reach the small intestine. When the pancreas is inflamed, the digestive enzymes attack the tissues of the pancreas.
Gallstones
Some studies have shown that smoking may increase the risk of developing gallstones. However, research results are not consistent and more study is needed.
Gallstones are small, hard particles that develop in the gallbladder, the organ that stores bile made by the liver. Gallstones can move into the ducts that carry digestive enzymes from the gallbladder, liver, and pancreas to the duodenum, causing inflammation, infection, and abdominal pain.
It’s never too late to quit!
Quitting smoking can reverse some of the effects of smoking on the digestive system. For example, the balance between factors that harm and protect the stomach and duodenum lining returns to normal within a few hours of a person quitting smoking. The effects of smoking on how the liver handles medications also disappear when a person stops smoking. However, people who stop smoking continue to have a higher risk of some digestive diseases, such as colon polyps and pancreatitis, than people who have never smoked.
Quitting smoking can improve the symptoms of some digestive diseases or keep them from getting worse. For example, people with Crohn’s disease who quit smoking have less severe symptoms than smokers with the disease.
A healthy diet and lifestyle, along with making smart healthcare decisions, can be a pathway to a healthier heart. Your family history can have some impact on your chances of heart disease, but there are some simple steps one can follow that, if you stick to them, can offer long-term heart-health benefits.
The American Heart Association notes that a heart-healthy diet should include:
Make sure the foods you eat are “heart healthy.” Include foods high in fiber, such as oat bran, oatmeal, whole-grain breads and cereals, fruits and vegetables. Cut back on foods high in saturated fat or cholesterol, such as meats, butter, dairy products with fat, eggs, shortening, lard and foods made with palm oil or coconut oil. Limit foods with trans fat, such as snack foods and commercial baked goods. Limit saturated fat, trans fat, sodium, red meat, sweets and sugar-sweetened beverages. If you choose to eat red meat, select lean cuts.
Use up at least as many calories as you take in. Find out how many calories you should be eating and drinking to maintain your weight. Nutrition and calorie information on food labels is typically based on a 2,000-calorie diet. You may need fewer or more calories depending on your age, gender and level of physical activity. Control your calories through portion control. Eat until you are comfortably full but not stuffed. If you eat out, this can lead to yummy leftovers.
If you aren’t sure how to eat right, ask us about our new Creative Pharmacist program. We can help you with planning meals to help lower fat and calorie content in your diet to reach and maintain a healthy weight. This program also provides specific exercises tailored to your specific goals.
Lifestyle choices are important. Smoking significantly increases your chance for heart disease. If you smoke, quit. Your doctor can tell you about ways to help you quit smoking. Try to avoid even secondhand smoke. And avoid drinking too much alcohol. This can raise your blood pressure and increase your risk of heart disease.
Regular exercise can help you maintain your weight, keep off weight that you lose and help you gain greater cardiovascular fitness. Each week, try to get at least 150 minutes of moderate physical activity, 75 minutes of vigorous physical activity or an equal combination of both. Aim for at least 30 minutes of exercise most days of the week. Sounds like a lot for you? This is easier than you think! Take a half-hour walk every day. Or walk for 10 minutes after each meal. Use the stairs instead of the elevator. And park at the far end of the lot. If you are not able walk for long periods of time or take the stairs, talk to your doctor about other exercises that will work for you.
If you don’t know your numbers for cholesterol, blood pressure or blood sugar, make an appointment with your doctor and have them checked. Your healthcare provider should test your blood levels of cholesterol at least once every five years. If you have already been diagnosed with high cholesterol or have a family history of the condition, you may need to have your cholesterol checked more frequently.
If you have high cholesterol, high blood pressure, or diabetes, you can take steps to lower your risk for heart disease. These can be diet or lifestyle changes, and/or medications prescribed by your doctor.
Ask your doctor whether you should take an aspirin every day. Studies have shown that taking a low dose of aspirin every day can help reduce your risk of heart disease and stroke.
BMI
Your Body Mass Index (BMI) is the number used to assess if you are underweight, normal weight, overweight, or obese. It is calculated using your height and weight and is a good gauge for the risk of diseases that can occur with more body fat. The higher your BMI, the higher your risk for diseases such as heart disease, high blood pressure, type 2 diabetes, gallstones, breathing problems, and certain cancers. The recommended range is 18.6 x 24.9.
Although BMI can be used for most men and women, it does have some limits:

Blood Sugar
Blood sugar, or glucose, is the main sugar found in your blood. It comes from the food you eat, and is your body’s main source of energy. Your blood carries glucose to all of your body’s cells to use for energy. When your blood sugar levels are too high, it causes diabetes. Over time, diabetes can cause other health problems and put you at higher risk for heart disease. A healthy blood sugar level should be less than 100 following an 8-hour fast.
Waste Size
Having extra body fat around your stomach increases your risk of heart disease and diabetes. The target for women is less than 35” and for men less than 40”.
Blood Pressure
High blood pressure has no warning signs or symptoms, and many people do not know they have it. So, it’s important to measure your blood pressure regularly. It is quick and painless, and it is the only way to know whether your pressure is high. You can check your blood pressure at a doctor’s office, at a pharmacy, or at home.The top number (Systolic) should be under 130. The bottom number (Diastolic) should be under 80.
Cholesterol
Did you know that 1 in 3 American adults has high cholesterol? Are you one of them? Too much cholesterol puts you at risk for heart disease and stroke, two leading causes of death in the United States. High cholesterol has no signs or symptoms, so the only way to know if you have it is to get your cholesterol checked.
Schedule an appointment and talk to your doctor about your all of your numbers and how they impact your overall health.